Fragile X syndrome begins developing even before birth
Fragile X syndrome (FXS), the most common form of inherited intellectual disability, may be unfolding in brain cells even before birth, despite typically going undiagnosed until age 3 or later. These results could fundamentally change how scientists understand the developmental origins of fragile X syndrome and suggest a potential treatment for brain cells damaged by the dysfunction.

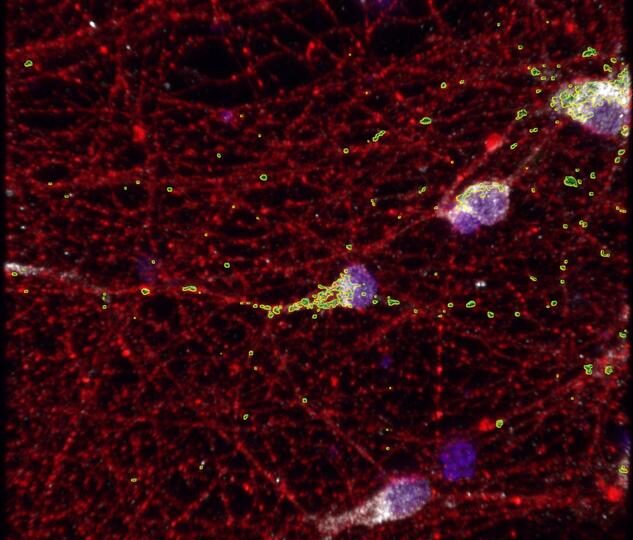
Mitochondria (shown in green) aren’t working as they should in the neurons (shown in red) of people with FXS. Researchers have identified a gene involved in this mitochondrial dysfunction, as well as a potential treatment. ©Minjie Shen, University of Wisconsin–Madison.
Individuals with FXS may present developmental delays — not sitting, walking or talking at expected ages — as well as mild to severe intellectual disability, learning disabilities and social and behavioral problems. About half are also diagnosed with autism spectrum disorder. A new study published in Neuron by researchers at the University of Wisconsin–Madison showed that FMRP, a protein deficient in individuals with FXS, has a role in the function of mitochondria during prenatal development. The study, led by four postdoctoral fellows — Minjie Shen, Carissa Sirois, Yu (Kristy) Guo and Meng Li — working in the lab of Xinyu Zhao, found that FMRP is regulating RACK1(Receptor for Activated C Kinase 1) gene to promote mitochondrial function. Using a drug to enhance mitochondrial function, they were also able to rescue brain cells damaged by lack of FMRP.
FMRP regulates essential genes
In previous research, Zhao found that mitochondria in mice with an FMRP deficiency that imitates FXS were smaller and unhealthy. Diving deeper, they also discovered that FMRP regulates genes involved in mitochondria fission-fusion, a process into which mitochondria fuse into a bigger shape in order to produce more energy for the cell. For the study, researchers grew FXS patient stem cell-derived neurons to study whether mitochondria in human cells experienced issues similar to those in mice. “And indeed, we found that human neurons also have fragmented mitochondria,” Zhao says. They also found fewer mitochondria in neurons derived from FXS patients, which they did not see in the neurons of the mice modeling FXS. “In human neurons, it’s a deficit in twofold. Not just fission-fusion, but also likely in the production of mitochondria,” Zhao says. Although it has been long known that FMRP is deeply involved in FXS, the new discovery pinpoints a role for the protein in early development of the condition. Symptoms of FXS present long after the baby is born. Many babies appear to be developing typically before showing slower development, autistic features or developmental deficits. Children with FXS are typically diagnosed at three years of age or older. “Which means many scientists have been thinking that FMRP is more important for the postnatal maturation state,” Zhao says. FMRP regulates the use of mRNA, and the researchers found that many of the mRNA strands that interact with FMRP are implicated in autism, providing a molecular link between FXS and autism spectrum disorder. Unexpectedly, many FMRP-bound mRNAs are expressed by genes classified as essential — genes that are very busy during prenatal development but less active after birth. “This means that FMRP has a function in prenatal development that we have not really thought about before,” Zhao says. “The fact that we found that FMRP also regulates prenatal development is really interesting and is actually indicating that what we see in fragile X syndrome, some of the effects already happened within the prenatal development.”
RACK1, a new target for the treatment of FXS?
One of those essential genes is RACK1, identified for the first time as playing a role in FXS. “When RACK1 is lower in fragile X neurons, the mitochondria are suffering and the neurons exhibit mitochondrial deficit and hyperexcitability, like immature neurons. But when we reintroduce RACK1, we can rescue this,” Zhao says. Using cultured neurons derived from individuals with FXS to screen for drugs, the researchers found that leflunomide corrected mitochondrial deficits. The treatment improved mitochondrial function and reduced the neurons’ hyperexcitability. Next, Zhao wants to do a detailed biochemical analysis of mitochondrial dysfunction and figure out which key proteins are less present in FXS-affected neurons. She is also working on better understanding how RACK1 and leflunomide work to rescue mitochondrial function. These results could fundamentally change how scientists understand the developmental origins of fragile X syndrome and suggest a potential treatment for brain cells damaged by the dysfunction.
Species-specific FMRP regulation of RACK1 is critical for prenatal cortical development. Minjie Shen et al. Neuron https://doi.org/10.1016/j.neuron.2023.09.014
11/10/2023



COMMENTS ARE OFF THIS POST