New technology allows molecules to enter cells safely
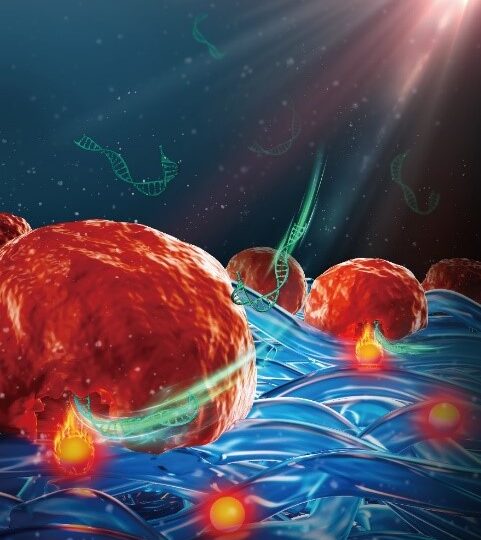
Professor Braeckmans from Ghent University focused the last ten years on a method for safe engineering of therapeutic cells with photothermal nanofibers. Now, Nature Nanotechnology gives insight in how these biocompatible photothermal nanofibers were developed, and how, upon laser irradiation, cells that come in contact with those nanofibers become permeabilized and can be transfected with a variety of effector molecules, including CRISPR/Cas9 ribonucleoprotein complexes and siRNA. Professor Braeckmans and his team demonstrated that cells, such as embryonic stem cells and human T cells, transfected with such nanofibers are in excellent health and retain their therapeutic functionality.
New basis for cell-based therapies

Cells on photothermal nanofibers become permeabilized and transfected upon laser irradiation
Cell-based therapies constitute a newer form of treatment in which genetically modified cells are injected in patient in order to prevent or treat illnesses. A well-known example is the use of a cancer patient’s own immune cells which can be isolated, genetically modified and expanded in a lab environment, and reinfused into the patient to attack the tumor cells. Genetic modification of cells depends on intracellular delivery technologies which often struggle with obtaining sufficient efficiency while having minimal impact on the cell’s health and functioning.
Nanoparticle-sensitized photoporation is particularly promising in this regard as it typically provides high efficiency, high throughput and low toxicity. It is based on the use of light-responsive nanoparticles, such as gold nanoparticles (NPs), which can form explosive nanobubbles upon pulsed laser irradiation. Those tiny explosions can induce small pores in cell membranes, allowing external effector molecules supplemented in the cell medium to enter cells. However, translation of nanoparticle-sensitized photoporation to clinical applications is hindered by the fact that cells have been in contact with (non-degradable) nanoparticles, posing toxicological and regulatory concerns.
Therefore, a new approach is needed that retains the advantage of nanoparticle-sensitized photoporation while avoiding direct contact of nanoparticles and cells. As shown in Figure 2, professor Braeckmans and his team embedded photothermal iron-oxide nanoparticles (IONPs) into biocompatible polymeric nanofibers which were produced by electrospinning. Polycaprolacton (PCL) is a biocompatible polymer widely used in biomedical applications, while IONPs are cost efficient and have a broad light absorption spectrum.

They show that both adherent and suspension cells can be safely and efficiently transfected with a range of macromolecules upon irradiation with nanosecond laser pulses. By performing elemental analysis via inductively coupled plasma – tandem mass spectrometry (ICP-MS/MS), they confirm that IONPs remain safely embedded in the nanofibers after laser irradiation so that the treated cells are effectively free from direct exposure to nanoparticles. Numerical simulations on heat transfer from fiber-embedded IONPs to nearby cells were performed to better understand how the laser pulse fluence, IONP distribution and aggregation state influence cell membrane permeability.
Experimentally the team showed that photoporation with photothermal nanofibers could successfully deliver functional biological molecules, including siRNA or CRISP-Cas9 ribonucleoproteins (RNPs), to both adherent and suspension cells, including human embryonic stem cell (hESC) and primary human T cells. As a benchmark a comparison was performed with state-of-the-art electroporation. While electroporated cells suffered from changes to their phenotype and functionality, this was not the case for photoporated cells who retained their capacity to proliferate and, in case of CAR-T cells, to kill tumor cells. Finally, PEN photoporation was used to transfect CAR-T cells with siRNA targeting the PD1 receptor, a well-known immune checkpoint inhibitor. siPD1 treated cells were confirmed to have enhanced tumor killing capacity in vivo.
Together it shows that photoporation with photothermal nanofibers enables efficient and safe intracellular delivery of a broad range of effector molecules in a variety of cell types without contact to potentially toxic photothermal nanoparticles. “We believe this is an important step towards the use of photoporation for safe and efficient production of gene modified cell therapies,” says professor Braeckmans.
Xiong, R., Hua, D., Van Hoeck, J. et al. Photothermal nanofibres enable safe engineering of therapeutic cells. Nat. Nanotechnol. (2021). https://doi.org/10.1038/s41565-021-00976-3
25/10/2021



COMMENTS ARE OFF THIS POST